Payer Intelligence to Gather Feedback and Understand Potential Coverage and Reimbursement of an AI CVD Technology
Case Study:
Exploring Coverage Potential for an AI-Driven CVD Diagnostic Platform
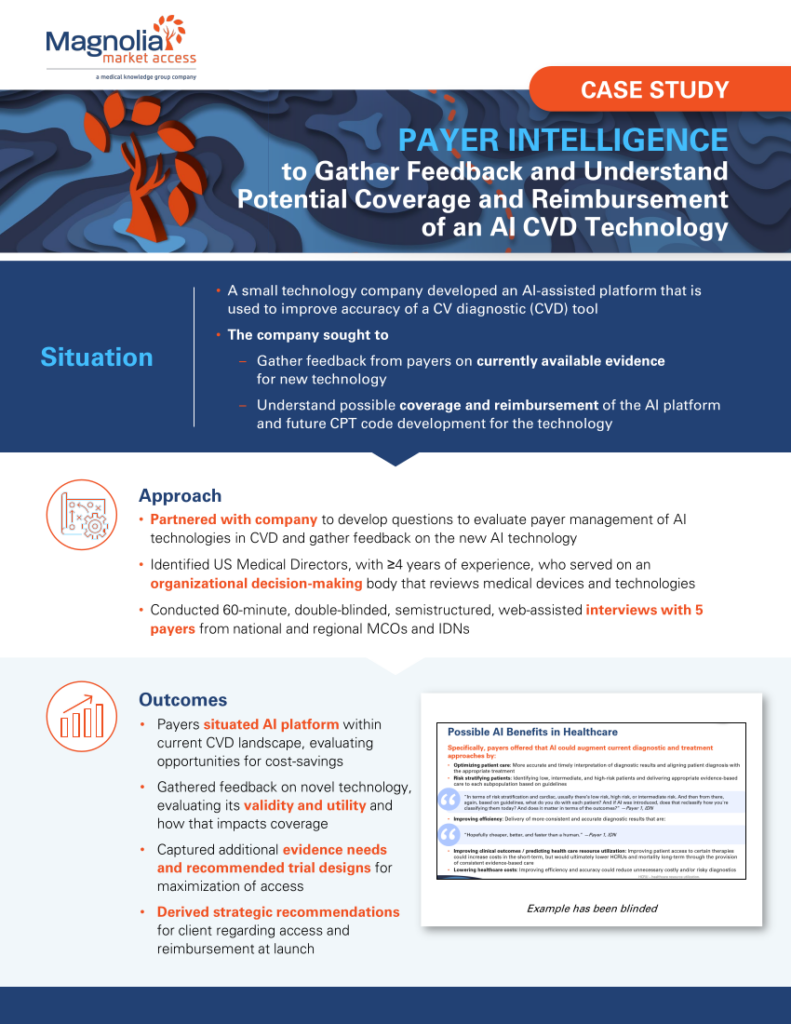
This case study illustrates how a technology company gained critical insights into payer perspectives and potential reimbursement strategies for a novel AI-assisted cardiovascular diagnostic (CVD) tool.
Key highlights include:
- Challenge: Understand payer feedback on the clinical evidence for the AI platform and explore potential coverage and reimbursement pathways.
- Approach: Magnolia conducted 60-minute interviews with experienced medical directors from national and regional managed care organizations (MCOs) and integrated delivery networks (IDNs) to evaluate the technology’s landscape, validity, and cost-saving opportunities.
- Outcome: Insights into payer expectations, evidence gaps, and recommended trial designs informed strategic recommendations for access and reimbursement at launch.
Download the case study to learn how payer intelligence can guide innovative technology adoption and maximize market access.